Many patients who have recovered from COVID-19 report continued fatigue and forgetfulness; a condition being described as the COVID-19 brain fog. Now that the COVID-19 pandemic has unfortunately been a part of our lives for over a year, healthcare professionals are noticing that some patients have developed persistent symptoms.
Actually, the concept of continuing and nagging symptoms after a viral infection is not a new occurrence- scientists have already coined this term Post-Viral Fatigue Syndrome, or PVFS. It has been recorded in patients that have recovered from other illnesses, such as the Epstein Barr virus (the virus that causes mononucleosis), and has even been noted in those that recovered from the ‘original’ SARS-COV1 virus in 2002-2003.
In most cases some degree of post-viral fatigue occurs but is short-lived and there is normally a steady return to normal health and activity levels over a period of a few weeks. However, when the symptoms plateau and persist for more than 3-4 months, a person can then be diagnosed with PVFS.
What is Brain Fog?
One of the most prominent symptoms seen with PVFS is something called “brain fog”. You may have heard this term thrown around, but what exactly is brain fog? Admittedly, this is a newer medical term that many doctors are not entirely familiar with yet, and we all could certainly benefit from some education regarding the same. Brain fog is a type of cognitive dysfunction (i.e., the brain’s thinking processes are not working correctly or efficiently) and often involves problems in short-term/working memory, concentration, and information processing.
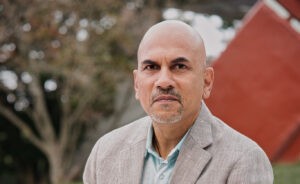
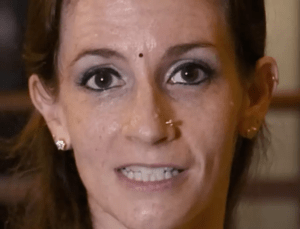
Often, symptoms are worsened after one exerts themselves (when attempting exercise, or simply after a long workday) or if they have not had a proper sleep the night before. Brain fog can therefore be confused with more common and better-studied disease states such as depression, anxiety, ADHD, anemia, or obstructive sleep apnea. It is important to recognize the subtle differences to avoid mismanagement and unnecessary medications, explained Dr. Jennifer Prabhu M.D., FAAP, FACP, MT(ASCP) CEO and co-founder of Circee Health, Pvt. Ltd
What percentage of Covid19 patients are facing brain fog?
Dr. Prabhu said, “Scientists currently estimate (although more studies and data are needed) that as many as 10-12% of COVID-recovered patients will develop symptoms of PVFS. Reassuringly, more than 35% of COVID-19 patients will experience some sort of residual fatigue, but this lasts less than 3 weeks post-infection. It is important to also remember that lack of a positive COVID-19 test (and in the same vein, the presence of a negative test) certainly does not rule out this syndrome. Therefore, please understand that, as with many other post-viral or bacterial syndromes, antiviral, antibiotic or medications will NOT cure these symptoms! The virus has already left the body, and it’s after-effects are now the problem.”
What are the signs and symptoms?
I have mentioned some of the symptoms of brain fog above. At the moment, the consensus of most researchers is that, in order to establish a diagnosis of PVFS, the following criteria must be present: post-exertional muscle fatigue and/or general malaise, symptom exacerbation after exercise, and all or most of three core symptoms: cognitive dysfunction/brain fog, unrefreshing sleep and orthostatic intolerance (feeling dizzy or giddy when changing position quickly). These symptoms should have persisted for more than 3 months and will have caused a substantial impact on the person’s ability to complete his or her normal daily activities.
Perhaps even more important than meeting these aforementioned criteria, other medical explanations for chronic fatigue should have been excluded (via thorough physical examination and laboratory evaluation), explained Ms. Jennifer.
How healthy lifestyle habits can help boost your mental function?
Dr. Prabhu, Thankfully, as the causes and features of this syndrome become more clear, so have potential preventive measures, treatments, and ameliorating lifestyle changes. Perhaps the most important first step in the treatment of any form of PVFS and the associated brain fog involves good old-fashioned convalescence – a fancy medical term for rest! In fact, many of these patients have been advised by their physicians to actually schedule naps/rest periods throughout the day and allow for longer nighttime sleep periods. One should also try to avoid any known stressors (both physical and emotional) to allow your brain and body to truly recover.
Gentle and daily physical exercise should be phased in once an effective sleep and nap routine has been established. Meditation, pranayam and yoga should also be encouraged, as tolerated. And, of course, with recovery from any illness, proper hydration (at least 2-3L of water a day) and a healthy diet is paramount- concentrate on whole foods (not processed) and plant-based (avoid meat, fish, dairy and eggs) meals.
Finally, a few supplements are being studied to see if they can also mitigate symptoms- Coenzyme Q10, 600mg/day, Magnesium glycinate 400mg/night, Zinc 50mg/day, Vitamin C 1000mg/day, and Melatonin 0.3-2mg at night. You may recognize these supplements as those that have also been recommended for COVID-19 prevention and treatment- it’s not a coincidence!
Just to reiterate, this phenomenon only occurs in a small percentage of COVID-19 victims, and the exact mechanisms are still not well known. As always, please consult with your family physician before confirming the diagnosis or beginning any of the above treatment regimens. Although, it never hurts to take this opportunity to consider improving your health with a cleaner diet and more efficient exercise and recovery!
As reported in the following news outlets (click to visit):